
2023 State of the Market - Employee Benefits
NOTE: Discover valuable insights on 2024 insurance market conditions. For a detailed analysis and comprehensive information, visit our State of the Insurance Market | 2024 Initial Outlook.
Industry Insights
Employee Benefits continues to be an increasingly complex area, with costs rising from multiple directions and recruitment and retention strategies dynamically shifting.
In 2023, organizations will need to have sound strategies to balance costs with employees’ needs and expectations.
Economic worries will continue to fuel cost sensitivity
 Employer benefits costs are impacted by rising medical plan costs, higher short- and long-term disability rates due to extended COVID-related illness and recovery periods, and inflation. While some industries are seeing layoffs, many continue to experience talent shortages. This, along with needing to prioritize employee wellbeing coming out of the pandemic, means employers cannot shift costs to their employees as they may have done in pre-pandemic years.
Employer benefits costs are impacted by rising medical plan costs, higher short- and long-term disability rates due to extended COVID-related illness and recovery periods, and inflation. While some industries are seeing layoffs, many continue to experience talent shortages. This, along with needing to prioritize employee wellbeing coming out of the pandemic, means employers cannot shift costs to their employees as they may have done in pre-pandemic years.
Rising pharmacy costs from multiple pressure points
New technologies and treatments have accelerated the expense associated with specialty medications. A strong pipeline of new specialty drugs coupled with the emergence of effective gene-specific therapies has further hastened a rise in costs which can be meteoric for some life-saving genetic treatments.
A lesser-known pharmacy pressure point is existing drugs with greatly expanded uses backed by newer clinical evidence. Rather than the usual suspects of specialty medications alone, these higher-cost brand medications for chronic diseases are also making waves.
For example, newer FDA-approved drugs developed to treat type 2 diabetes are poised to dominate a second major health condition: obesity. This opens the door for greater prescriber use for many more patients. As well, patient demand for these drugs has exploded with heavy influence from manufacturer strategic marketing, social media, and investigative television shows.
This trend presents challenges such as:
- Increased off-label use outside the intended treatment population
- Impacts through the spillover trend in diabetes for employers (plan sponsors) who do not elect weight-loss coverage under their pharmacy benefit
Changing recruitment and retention dynamics critical to consider
Employers are facing another year of uncertainty and complexity while also having to manage the threat of a recession. These headwinds continue to complicate matters for the most seasoned executives and their ability to plan for and meet operational and growth targets, let alone thrive. And, even with some industries and organizations engaging in sweeping layoffs, competition for top staff and executive talent remains a concern for organizations.
Competitive pay and a comprehensive employee benefits program have long been recruitment and retention drivers. Employees are now seeking a more personalized employment experience. In the modern, diverse workplace, one-size-fits-all benefits are not enough.
Strategic employers continue to expand beyond traditional benefits such as medical, dental, vision, life insurance, disability coverage, and retirement programs to offer benefits that support the employee’s overall quality of life. These benefits range from flexible work arrangements to mental, physical, and financial wellbeing programs, to paid volunteer time off, and more.
Coverage Considerations
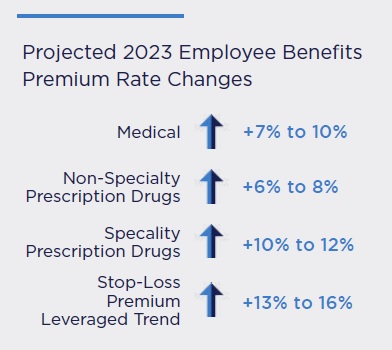
Health plan costs are expected to increase between 7-10% in 2023. While healthcare costs rise every year, current medical trend predictions reflect a six to 12-month lag, meaning costs will rise more than current predictions indicate. Many expect costs to increase further in the next few years as impacts of inflation begin to bear out across the healthcare marketplace. Inflation in healthcare lags general inflation because of the multi-year agreements prevalent in health plan contracts between insurers and providers.
Stop-loss premiums will also climb 13–16% to match healthcare cost escalations. Employers will continue to experience ‘lasers’ where coverage for a specific claimant is adjusted by raising their individual deductible to mitigate risk. The financial exposure is ultimately shifted to the plan sponsor.
These trends point to the need to “optimize” — to control costs while also managing rapidly changing workforce needs and expectations. Employers must:
- Uncover the inefficiencies in their healthcare programs that data can reveal and use the data to drive programmatic changes.
- Explore all possible options for efficiently financing their healthcare spend through alternative funding models.
- Keep retention in focus by being aware of the heightened sense the workforce has for health support, and the impact of inflation on their own healthcare costs.
In an environment where employers are dealing with rising costs and an uncertain economic outlook, interest in managing long-term costs has become a priority. Striking the right balance between a diverse workforce’s needs and managing and mitigating risks such as those that come with large claims is key to seeing the way forward with an employee benefits strategy.
"In an environment where employers are dealing with rising costs and an uncertain economic outlook, interest in managing long-term costs has become a priority."
Recommendations
Use data analytics to make healthcare determinations that reduce costs while providing the best care for staff
It is essential for employers to carefully steward their healthcare benefits dollars in this environment. They must understand the inefficiencies in their healthcare programs and use data analytics to drive programmatic changes. Data analytics can help organizations use demographic and claim data to:
- Identify and engage high-cost members. Because most healthcare costs are borne by a small number of plan members, management of these members can have an outsized impact on overall spend. Using predictive analytics to identify and engage these members earlier can significantly reduce costs.
- Ensure appropriate health management programs. Without visibility and analysis of claims, employers risk using resources on programs inappropriate for their population. For example, investing in family planning benefits when the claims indicate higher incidences of diabetes and related comorbidities would be a lost opportunity.
- Steer employees to high value providers. The recent efforts to make the cost of care more transparent to all stakeholders presents an opportunity to socialize the importance of healthcare quality. High-quality providers often cost less than low-quality providers, as the latter results in greater complications, readmissions, and the like. By leveraging cost and quality data, employers can design high-performance-only network plan options, emphasize centers of excellence, and steer employees to high value providers and proper sites of care. Doing so will provide plan cost savings and a better healthcare experience for plan members.
Design the Employee Benefits portfolio that is right for your business
While broader choice is directionally appropriate for most organizations, this does not mean offering a plethora of options is right for your business or for your employees. The Great Resignation and changing workforce expectations and demographics mean most employers need to consider how those dynamics impact their ability to staff at all levels and keep those staff engaged.
Long-term benefits planning and a regular check-and-adjust strategy is critical to that end.
